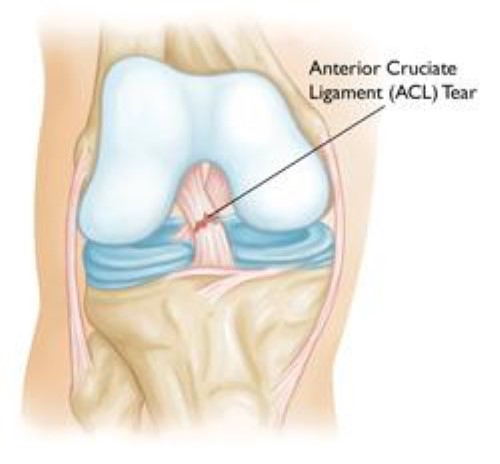
An ACL tear is used to describe any injury to the Anterior Cruciate Ligament. Most commonly, the ACL pulls away from its origin on the end of the thighbone. It may also simply stretch or only be "partially" injured.
ACL tears are one of the most frequently talked about sports injuries. They are one of the most common knee injuries. It is estimated that about 200,000 occur in the US each year. As sports become more competitive in adolescent and female athletes, these groups have seen an increase in ACL tear frequency. Infact, ACL tears are approximately 3 times more frequent in females and about 5% of year-round female soccer and basketball players will sustain an ACL tear.
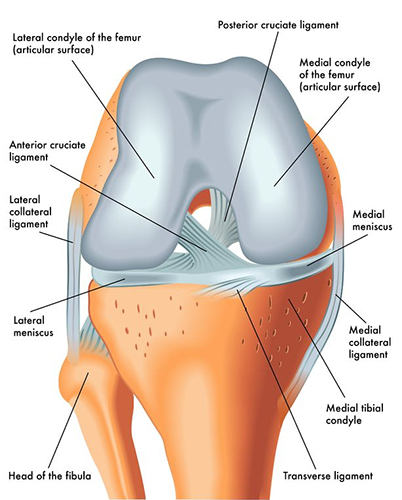
Ligaments are thick firm bands of tissue that connect one bone to another. The ACL is one of the four major ligaments in the knee. The ACL and the three others (PCL, MCL, LCL), connect the bottom of the thigh bone (femur) and the top of the shin bone (tibia). By doing so, these ligaments stabilize the knee. The ACL is primarily responsible for preventing excessive back to front motion of the tibia on the femur and rotation of the tibia outwards. When there is an ACL tear, the ACL is unable to prevent these motions and the knee will often feel unstable. This instability will typically be felt during pivoting, cutting and jumping activities. Some, however, may have instability with everyday non-sport activities.
Most often an ACL tear will occur during a non-contact pivoting or jumping activity, such as during skiing, team sports or racquet sports. Often the injury will occur while engaging in an activity that has frequently been performed in the past without injury.
Occasionally an ACL tear will occur from direct contact to the knee. ACL tears caused by contact are often associated with additional ligament injuries. Even more rarely, an ACL tear may occur from a simple slip or fall while performing everyday non-sport activities, such as those that may occur when stumbling on a wet surface or while dancing.
There are a number of potential risk factors for ACL tears. Those often discussed are: fatigue, activity intensity (game vs. practice), field surface, shoe type, jumping and landing techniques, size and shape of particular areas of the knee, female sex and associated female hormonal status.
Pop! Ouch! No its not an old Batman episode. If you were playing a team or racquet sport. Or were skiing and fell. Chasing your kids while playing tag. Or simply dancing. If you felt a painful "pop" and you had to stop the activity. Your knee then began to swell and become stiff. Unfortunately, you likely have a torn ACL (Anterior Cruciate Ligament.
The ACL is one of the four major ligaments of the knee. It's in the center of the knee and connects the end of the thighbone to the top of the shin bone. It provides stability to the knee and its presence is critical for pivoting, cutting or landing from a jump. After a torn ACL, participating in racquet sports, team sports, hiking, dancing and any other sports or activities that require those skills is difficult as well as dangerous to the knee.
The most common symptoms of an acutely torn ACL are:
All of these symptom are not always present when the ACL tears. However, an acute injury must occur. Without one, the ACL cannot be torn. Usually there is a non-contact twisting injury. In the video, Derrick Rose tears his left ACL as he plants his left leg and cuts to his right.
Less commonly, ACL tears can occur from an injury involving direct contact to the knee such as during a football or soccer tackle or while getting hit by a car. These injuries are often more severe and frequently occur in conjunction with tears of other knee ligaments.
If you have had these symptoms, it is a good idea to see an Orthopaedic Sports Medicine doctor.
Your sports medicine doctor should begin by asking you questions about the injury, trying to elicit a history of the events or symptoms discussed above. To a well-trained sports medicine doctor, these findings would be very suggestive of a torn ACL. An exam can confirm the diagnosis. The doctor will often want to manually assess stability, not only to diagnose the torn ACL, but also to assess for other ligament injuries.
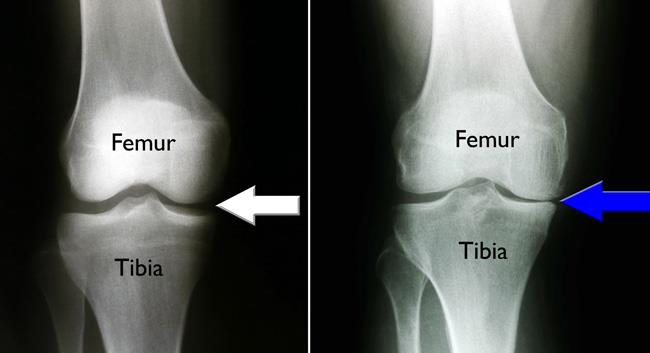
X-rays are often obtained to look for significant breaks in the bones. Fortunately, these rarely occur with most ACL injuries but even without a torn ACL, breaks can give many of the same symptoms and therefore must be ruled out.
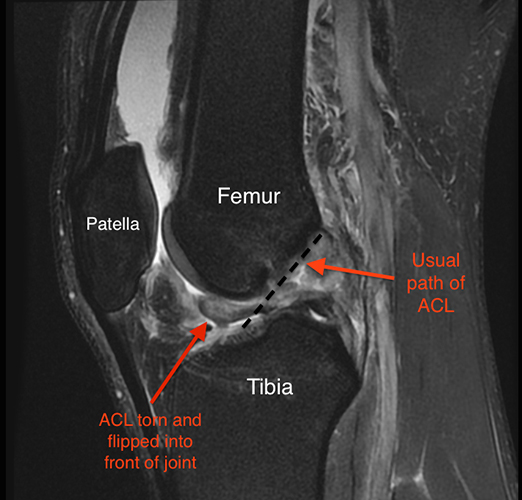
For a well-trained sports medicine doctor, a comprehensive history and exam and negative X-rays are often enough to make the diagnosis of a torn ACL and no other testing is needed. However, in this day and age, an MRI is usually obtained, not only to confirm the diagnosis but also to evaluate for injuries to the menisci, the cartilage on the ends of the bones around the knee and the remaining ligaments.
The ACL (Anterior Cruciate Ligament) is one of the four primary ligaments of the knee. It is critical in helping to stabilize the knee. Most often injuries occur during non-contact, pivoting activities. Typically there is immediate pain, often a noticeable "pop" or shift of the knee, an in ability to continue participating and subsequent stiffness and swelling. Although these early symptoms often resolve over 4-6 weeks, instability during athletic activities or any activities requiring cutting or jumping will persist. These episodes can then lead to further damage to the knee. For this reason, once you tear your ACL, treatment is necessary.
There really are only two good treatment strategies once you have torn your ACL:
Why is that? Well... For two reasons.
After an ACL tear, the knee will almost always be swollen, stiff and painful. This is not the time for torn ACL surgery. Surgery is inherently traumatic. Adding this trauma to the trauma from the injury, can lead to a "rocky" postoperative course :-( . After surgery performed too early, excessive stiffness can develop. This can sometimes require additional surgery to correct. For this reason, I, along with many of my colleagues, like to let the swelling, stiffness, pain and inflammation settle down before proceeding with torn ACL surgery. Usually about 4-6 weeks is required. Essentially, when the knee seems good enough that you feel surgery is not needed, that's when surgery should be considered.
Often patients would rather delay surgery to a time that better fits their schedule. Is this OK? Sure. ACL surgery is not emergent or even urgent. Of course delaying surgery assumes that you avoid all pivoting and jumping activities. As I mentioned above, involvement in these activities could result in further injuries and jeopardize the long-term status of your knee.
Take home messages:
Torn ACL surgery consists of a Reconstruction of the ACL (the ACL or a portion of the ACL is replaced) rather than a Repair (the injured ACL is sutured). Some of the basics of this procedure are:
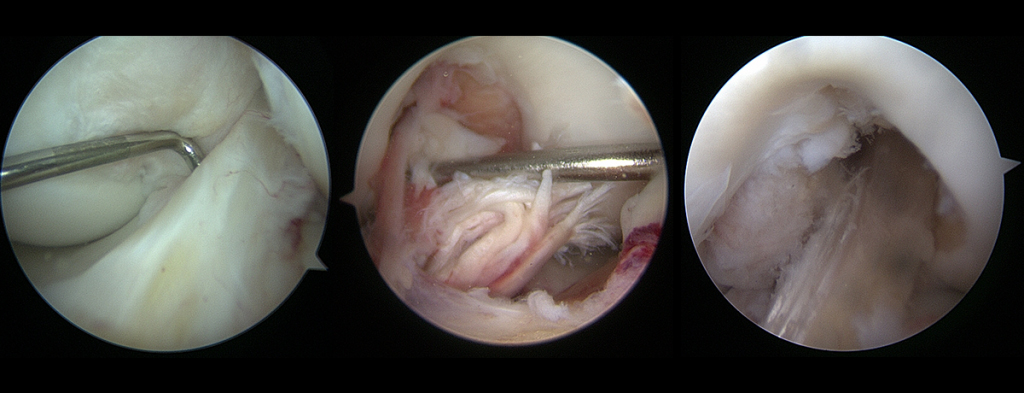
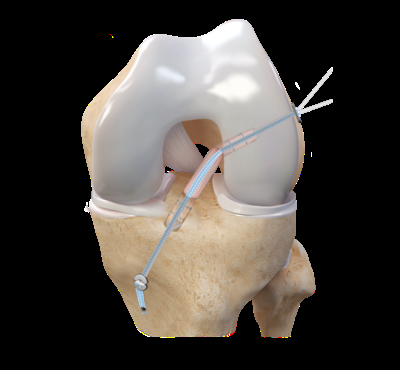
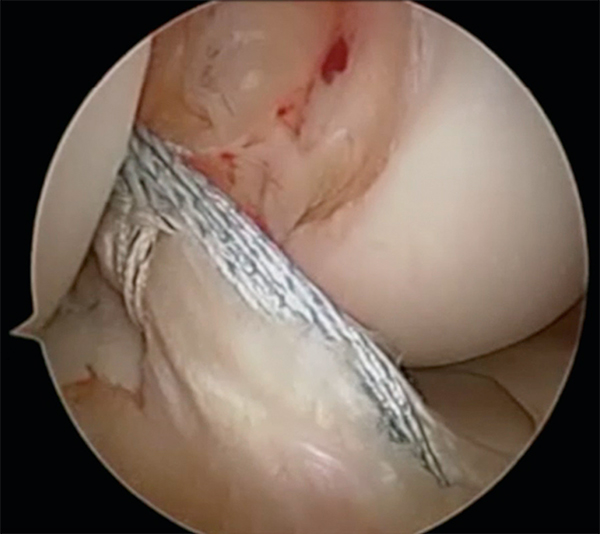
There are four potential grafts that may be used. They can be either autografts or allografts. Autografts come from the patient's knee. Allografts come from donors who have previously died. Like most things, each of the grafts have potential benefits and areas of concern. Which graft is best is based on a weighing of these variables.
We prefer Hamstring autografts for most of the torn ACL surgeries.
Different sports medicine surgeons may have different postoperative protocols after torn ACL surgery. For instance, on the occasion that I use an Allograft, because of concerns for slow "incorporation" and ultimate failure of the graft, I will slow down my postop program. Below I have detailed my usual postop regimen. You should discuss your recommended protocol with your surgeon.
These are only guidelines. I will often individualize this regimen based on symptoms, progress and other factors. There are a number of different ways, implants, technique to achieve the same results. Torn ACL surgery is no different.
Osteotomy literally means "cutting of the bone". In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped to relieve pressure on the knee joint.
Knee osteotomy is used when a patient has early-stage osteoarthritis that has damaged just one side of the knee joint. By shifting weight off of the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in an arthritic knee.
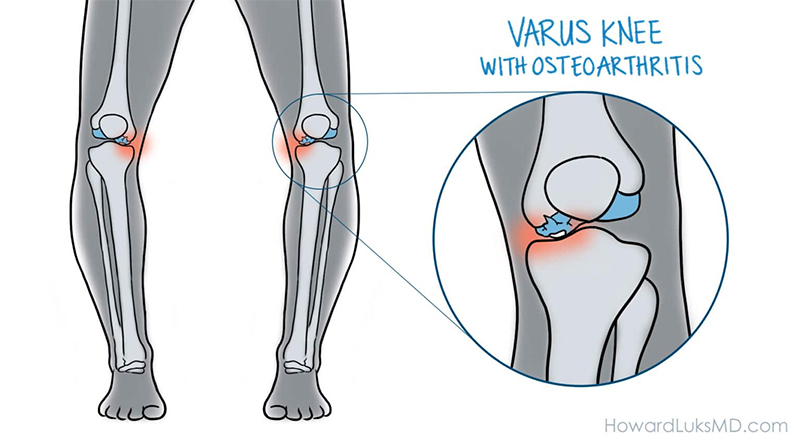
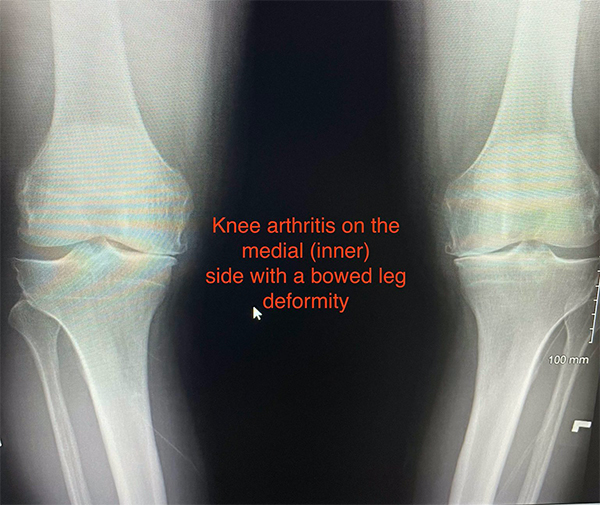
Osteoarthritis can develop when the bones of your knee and leg do not line up properly. This can put extra stress on either the inner (medial) or outer (lateral) side of your knee. Over time, this extra pressure can wear away the smooth articular cartilage that protects the bones, causing pain and stiffness in your knee.
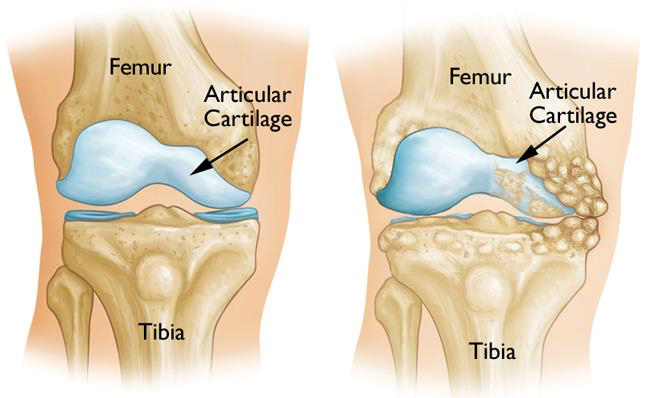
Knee osteotomy has three goals:
One advantage of the procedure is that, by preserving your own knee anatomy, a successful osteotomy may delay the need for a joint replacement for several years. Another advantage is that there are no restrictions on physical activities after an osteotomy - you will be able to participate in your favorite activities, even high-impact exercise. Osteotomy does have disadvantages. For example, pain relief is not as predictable after osteotomy compared with a partial or total knee replacement. And recovery from osteotomy is typically longer and more difficult because you may not be able to bear weight on your operated knee right away.
In some cases, having had an osteotomy can make later knee replacement surgery more challenging.
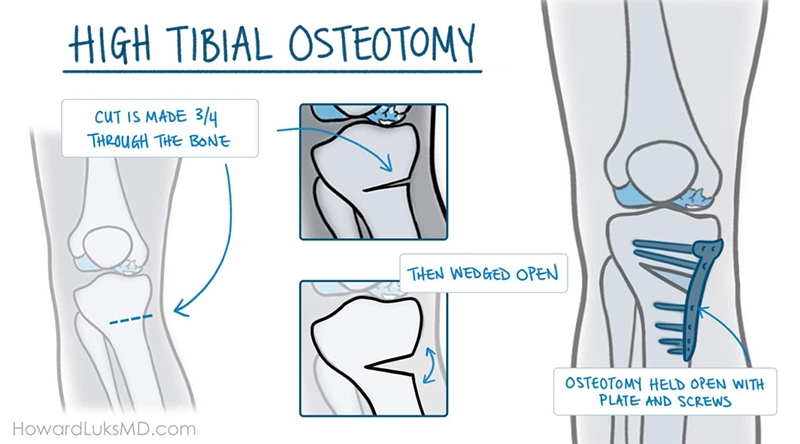
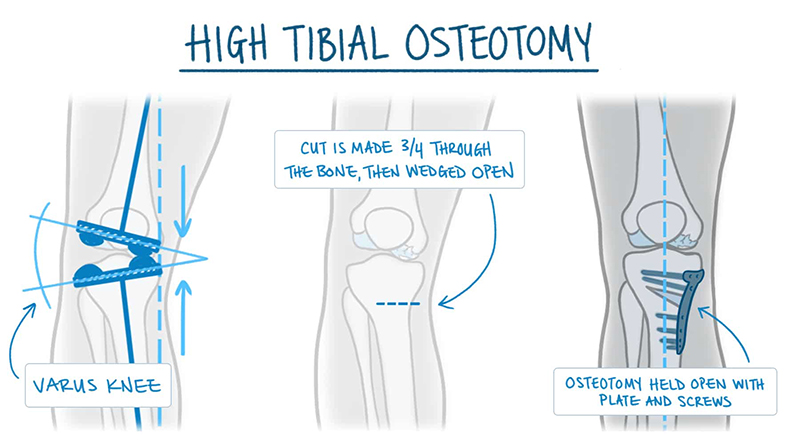
In a tibial osteotomy, a wedge of bone is removed to straighten out the leg. Most osteotomies for knee arthritis are done on the tibia (shinbone) to correct a bowlegged alignment that is putting too much stress on the inside of the knee.
During this procedure, a wedge of bone is removed from the outside of the tibia, under the healthy side of the knee. When the surgeon closes the wedge, it straightens the leg. This brings the bones on the healthy side of the knee closer together and creates more space between the bones on the damaged, arthritic side. As a result, the knee can carry weight more evenly, easing pressure on the painful side.
Tibial osteotomy was first performed in Europe in the late 1950s and brought to the United States in the 1960s. This procedure is sometimes called a "high tibial osteotomy". Osteotomies of the thighbone (femur) are done using the same technique. They are usually done to correct a knock-kneed alignment.
Knee osteotomy is most effective for thin, active patients who are less than 60 years old. Good candidates have pain on only one side of the knee, and no pain under the kneecap. Knee pain should be brought on mostly by activity, as well as by standing for a long period of time. Candidates should be able to fully straighten the knee and bend it at least 90 degrees. Patients with rheumatoid arthritis are not good candidates for osteotomy. Your orthopaedic surgeon will help you determine whether a knee osteotomy is suited for you.
You will likely be admitted to the hospital on the day of surgery. Before your procedure, a doctor from the anesthesia department will evaluate you. He or she will review your medical history and discuss anesthesia choices with you. Anesthesia can be either general (you are put to sleep) or spinal (you are awake, but your body is numb from the waist down).
Your surgeon will also see you before surgery and sign your knee to verify the surgical site.
After the wedge of bone is removed, the tibia may be held in place with a plate and screws.
A knee osteotomy operation typically lasts between 1 and 2 hours. Your surgeon will make an incision at the front of your knee, starting below your kneecap. He or she will plan out the correct size of the wedge using guide wires. With an oscillating saw, your surgeon will cut along the guide wires, and then remove the wedge of bone. He or she will "close" or bring together the bones in order to fill the space created by removing the wedge. Your surgeon will insert a plate and screws to hold the bones in place until the osteotomy heals.
This is the most commonly used osteotomy procedure, and is called a closing wedge osteotomy.
In some cases, rather than "closing" the bones, the wedge of bone is "opened" and a bone graft is added to fill the space and help the osteotomy heal. This procedure is called an opening wedge osteotomy.
After the surgery, you will be taken to the recovery room where you will be closely monitored as you recover from the anesthesia. You will then be taken to your hospital room.
As with any surgical procedure, there are risks involved with osteotomy. Your surgeon will discuss each of the risks with you and will take specific measures to help avoid potential complications.
Although the risks are low, the most common complications include:
In some cases, a second surgery may be required, particularly if the osteotomy does not heal.
Hospital discharge: In most cases, patients go home 1 to 2 days after an osteotomy.
Pain management: After surgery, you will feel some pain, but your surgeon and nurses will make every effort to help you feel as comfortable as possible. Many types of pain medication are available to help control pain, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs) and local anesthetics. Treating pain with medications can help you feel more comfortable, which will help your body heal faster and recover from surgery faster.
Opioids can provide excellent pain relief, however, they are a narcotic and can be addictive. It is important to use opioids only as directed by your doctor. You should stop taking these medications as soon as your pain starts to improve.
Weight bearing: After the operation, you will most likely need to use crutches for several weeks. Your surgeon may also put your knee in a brace or cast for protection while the bone heals. Your surgeon will give you instructions about when weight bearing can begin.
Doctor visit: You will see your surgeon for a follow-up visit after surgery. X-rays will be taken so that he or she can check how well the osteotomy has healed. After the follow-up, your surgeon will tell you when it is safe to put weight on your leg, and when you can start rehabilitation.
Rehabilitation exercises: During rehabilitation, a physical therapist will give you exercises to help maintain range of motion in your knee and restore your strength. You may be able to resume your full activities 3 to 6 months after surgery.
For most patients, osteotomy is successful in relieving pain and delaying the progression of arthritis in the knee. It can allow a younger patient to lead a more active lifestyle for many years. Even though many patients will ultimately require a total knee replacement, an osteotomy can be an effective way to buy time until a replacement is required.


